Home » History of Indian Medicine and Surgery
One of the earliest school of medicine known to mankind is Ayurveda. It was consolidated by Charaka nearly 2500 years ago. Sushruta, father of surgery, used to conducted complicated surgical procedures 2600 years ago, without the sophisticated instruments of today.
One of the earliest school of medicine known to mankind is Ayurveda. It was consolidated by Charaka nearly 2500 years ago. Sushruta, father of surgery, used to conducted complicated surgical procedures 2600 years ago, without the sophisticated instruments of today.
His principles, diagnoses, and cures retain their potency and truth even after a couple of millennium. When the science of anatomy was confused with different theories in Europe, Acharya Charak revealed the facts on human anatomy, blood circulation, embryology, pharmacology, and diseases like diabetes, heart disease, tuberculosis, etc.
In his book “Charak Samhita,” he has described the medicinal qualities and functions of 100,000 herbal plants. He has emphasized the influence of our diet and physical activities over our mind, which is even practiced by our today’s generation. He has proved the correlation between spirituality and physical health contributed greatly to diagnostic and curative sciences. He has also prescribed the ethical charter for medical practitioners two centuries prior to the Oath. Through his genius and intuition, Acharya Charak forever remains etched in the annals of history as one of the greatest and noblest of rishi-scientists.
His principles, diagnoses, and cures retain their potency and truth even after a couple of millennium. When the science of anatomy was confused with different theories in Europe, Acharya Charak revealed the facts on human anatomy, blood circulation, embryology, pharmacology, and diseases like diabetes, heart disease, tuberculosis, etc.
In his book “Charak Samhita,” he has described the medicinal qualities and functions of 100,000 herbal plants. He has emphasized the influence of our diet and physical activities over our mind, which is even practiced by our today’s generation. He has proved the correlation between spirituality and physical health contributed greatly to diagnostic and curative sciences. He has also prescribed the ethical charter for medical practitioners two centuries prior to the Oath. Through his genius and intuition, Acharya Charak forever remains etched in the annals of history as one of the greatest and noblest of rishi-scientists.
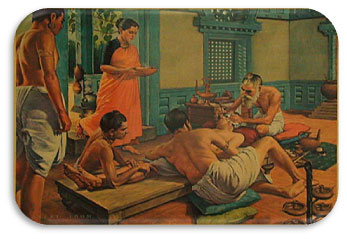
Cataract surgery and plastic surgery were also first performed by the ancient physician Sushruta. He used a curved needle and removed the cataract by pushing the lens. The eyes were then immersed in warm butter and were properly covered until they were completely healed. Usage of anesthesia was also well known in ancient India. People from far off countries came to India to seek treatment.
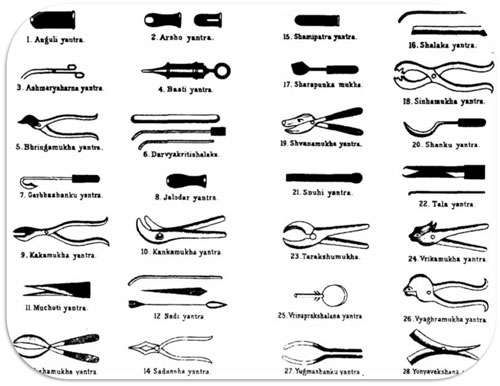
Born to sage Vishwamitra, Sushruta is the father of surgery. 2600 years ago, he along with the health scientists of his time conducted complicated surgeries like artificial limbs, cesareans, cataract, Rhinoplasty (restoration of a damaged nose), urinary stones, and 6 types of dislocations, 12 types of fractures, plastic surgery and even brain surgery. He is the author of the book “Sushruta Samhita”, in which he describes over 300 surgical procedures and 125 surgical instruments. Sushruta’s work was later translated into Arabic language and gradually passed on to European countries.
Also known as the science of longevity, Ayurveda is an ancient and traditional form of medicine that is not only prevalent today, but incredibly well-reputed and successful as well. The system of medicines is solely based on herbs and herbal compounds. Although Atreya and Agnivesa dealt with the principles of Ayurveda in 800 BC, Charaka Samhita is credited with the first Ayurvedic compilation. He was the first physician to posit the concepts of digestion, metabolism and immunity. He studied the human body and offered various remedies for numerous diseases.
Did You Know: A common misconception is that Indians use spices and herbs in their food to preserve it – however, this is only partly true. The herbs and spices actually form the basis of Ayurveda and were an effort to combine preventive medicine with everyday meals. Ayurveda dates back to 1st millennium BC, and laid the foundation for modern medicine.

Now while Ayurveda was flourishing up north, the south of India couldn’t rely on it because herbs were not available all year long. Hence, the Siddha Saints came up with their own solutions in 5 BC – the Siddha medicines. Rich and simple, the Siddha medicines were made from a combination of everyday spices and fruits, while also using certain metals, minerals and chemical products for the same.
Did You Know: Many of these medicines were also used to prevent bodies from decomposing, making it the first in the world to be used as a preservative.
Aptly called the “Father of Surgery”, Susruta was a great Indian surgeon who is credited with the book Susruta Samhita. In the book, he is said to have described over 300 surgical procedures and about 120 surgical instruments (all his own inventions). He also classified surgeries into eight categories for a better understanding. In the books, he has described every form of surgery – from bones, to tissues to various organs as well. He has also described the symptoms of diseases and offered prognosis for the same. His work was eventually translated and reached the Arab world, from where it was then transported to Europe many years later.
Did You Know: He made use of ant heads to hold skin together when stitching and substituted what we know as anaesthesia with wine!
While it may seem like a modern invention, Plastic Surgery was actually being carried out in India by 2000 BC. The method, they say, is not dissimilar to the method used today. In fact, some of the instruments and tools for surgery described in the book are still being developed in the 21st century.
The purpose of it back then was not nearly as aesthetic or superficial, it was more about improvement of deformed body parts, most notably ears, noses and using skin from other body parts for the same was a norm back in the day as well.
Cataract Surgery was first performed in India by, you guessed it, Susruta. The medical genius used a special tool called Jabamukhi Salaka which was used to loosen the lens and push the cataract out of the field of vision. The eye was later soaked with warm butter and bandaged. Although the method was successful and safe, Susruta said that these surgeries must be performed only when absolutely essential. In addition to that, the removal of cataract by surgery is credited to India as well.
Did You Know: The surgeries were so renowned that Greek philosophers and scientists travelled to India to observe these surgeries being performed by Susruta.
The practice of medicine changed in the face of rapid advances in science, as well as new approaches by physicians. Hospital doctors began much more systematic analysis of patients’ symptoms in diagnosis.[92] Among the more powerful new techniques were anaesthesia, and the development of both antiseptic and aseptic operating theatres.[93] Actual cures were developed for certain endemic infectious diseases. However the decline in many of the most lethal diseases was more due to improvements in public health and nutrition than to medicine.
Medicine was revolutionized in the 19th century and beyond by advances in chemistry and laboratory techniques and equipment, old ideas of infectious disease epidemiology were replaced with bacteriology and virology.[59]Germ theory and bacteriology
In the 1830s in Italy, Agostino Bassi traced the silkworm disease muscardine to microorganisms. Meanwhile, in Germany, Theodor Schwann led researches on alcoholic fermentation by yeast and proposed that they were alive—that is, microorganisms—a claim derided by leading chemists, such as Justus von Liebig, seeking solely physicochemical explanation, and alleging that Schwann’s was regressing to vitalism. In 1847 in Vienna, Ignaz Semmelweis (1818–1865), by requiring physicians to clean their hands before attending childbirth, dramatically cut new mothers’ death rate due to childbed fever, yet his principles were marginalized and attacked by professional peers.
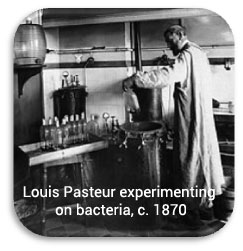
Starting in 1857 by confirming Schwann’s fermentation experiments, Louis Pasteur in France placed his eminent reputation behind the belief that yeast are microorganisms, and closed his paper by indicating that such process might also explain contagious diseases. In 1860, Pasteur’s report on bacterial fermention to butyric acid motivated fellow Frenchman Casimir Davaine to establish a similar species, which he called bacteridia, as the pathogen of the disease anthrax, costly to the cattle industry. Yet bacteridia were found inconsistently and dismissed as a disease byproduct, not cause. British surgeon Joseph Lister, however, already took cue and introduced antisepsis to wound treatment in 1865.
German physician Robert Koch, noting fellow German Ferdinand Cohn’s report of a spore stage of a certain bacterial species, traced the life cycle of Davaine’s bacteridia, identified spores, inoculated laboratory animals with them, and reproduced anthrax—a breakthrough for experimental pathology and germ theory of disease. Pasteur’s group added ecological investigations confirming spores’ role in the natural setting, while Koch published a landmark treatise in 1878 on the bacterial pathology of wounds. In 1881, Koch reported discovery of the “tubercle bacillus”, cementing germ theory and Koch’s acclaim.
Starting in 1857 by confirming Schwann’s fermentation experiments, Louis Pasteur in France placed his eminent reputation behind the belief that yeast are microorganisms, and closed his paper by indicating that such process might also explain contagious diseases. In 1860, Pasteur’s report on bacterial fermention to butyric acid motivated fellow Frenchman Casimir Davaine to establish a similar species, which he called bacteridia, as the pathogen of the disease anthrax, costly to the cattle industry. Yet bacteridia were found inconsistently and dismissed as a disease byproduct, not cause. British surgeon Joseph Lister, however, already took cue and introduced antisepsis to wound treatment in 1865.
German physician Robert Koch, noting fellow German Ferdinand Cohn’s report of a spore stage of a certain bacterial species, traced the life cycle of Davaine’s bacteridia, identified spores, inoculated laboratory animals with them, and reproduced anthrax—a breakthrough for experimental pathology and germ theory of disease. Pasteur’s group added ecological investigations confirming spores’ role in the natural setting, while Koch published a landmark treatise in 1878 on the bacterial pathology of wounds. In 1881, Koch reported discovery of the “tubercle bacillus”, cementing germ theory and Koch’s acclaim.
On losing the 1883 rivalry in Alexandria, Pasteur switched research direction, and introduced his third vaccine—rabies vaccine—the first vaccine for humans since Jenner’s for smallpox.[94] From across the globe, donations poured in, funding the founding of Pasteur Institute, the globe’s first biomedical institute, which opened in 1888.Along with Koch’s bacteriologists, Pasteur’s group—which preferred the term microbiology—led medicine into the new era of “scientific medicine” upon bacteriology and germ theory. Accepted from Jakob Henle, Koch’s steps to confirm a species’ pathogenicity became famed as “Koch’s postulates”. Although his proposed tuberculosis treatment, tuberculin, seemingly failed, it soon was used to test for infection with the involved species. In 1905, Koch was awarded the Nobel Prize in Physiology or Medicine, and remains renowned as the founder of medical microbiology.

Women had always served in ancillary roles, and as midwives and healers. The professionalization of medicine forced them increasingly to the sidelines. As hospitals multiplied they relied in Europe on orders of Roman Catholic nun-nurses, and German Protestant and Anglican deaconesses in the early 19th century. They were trained in traditional methods of physical care that involved little knowledge of medicine. The breakthrough to professionalization based on knowledge of advanced medicine was led by Florence Nightingale in England. She resolved to provide more advanced training than she saw on the Continent. At Kaiserswerth, where the first German nursing schools were founded in 1836 by Theodor Fliedner, she said, “The nursing was nil and the hygiene horrible.”
Britain’s male doctors preferred the old system, but Nightingale won out and her Nightingale Training School opened in 1860 and became a model. The Nightingale solution depended on the patronage of upper class women, and they proved eager to serve. Royalty became involved. In 1902 the wife of the British king took control of the nursing unit of the British army, became its president, and renamed it after herself as the Queen Alexandra’s Royal Army Nursing Corps; when she died the next queen became president. Today its Colonel In Chief is the daughter-in-law of Queen Elizabeth. In the United States, upper middle class women who already supported hospitals promoted nursing. The new profession proved highly attractive to women of all backgrounds, and schools of nursing opened in the late 19th century. They soon a function of large hospitals, where they provided a steady stream of low-paid idealistic workers. The International Red Cross began operations in numerous countries in the late 19th century, promoting nursing as an ideal profession for middle class women.
The Nightingale model was widely copied. Linda Richards (1841 – 1930) studied in London and became the first professionally trained American nurse. She established nursing training programs in the United States and Japan, and created the first system for keeping individual medical records for hospitalized patients. The Russian Orthodox Church sponsored seven orders of nursing sisters in the late 19th century. They ran hospitals, clinics, almshouses, pharmacies, and shelters as well as training schools for nurses. In the Soviet era (1917–1991), with the aristocratic sponsors gone, nursing became a low-prestige occupation based in poorly maintained hospitals.
Women as physicians
It was very difficult for women to become doctors in any field before the 1970s. Elizabeth Blackwell (1821–1910) became the first woman to formally study and practice medicine in the United States. She was a leader in women’s medical education. While Blackwell viewed medicine as a means for social and moral reform, her student Mary Putnam Jacobi (1842–1906) focused on curing disease. At a deeper level of disagreement, Blackwell felt that women would succeed in medicine because of their humane female values, but Jacobi believed that women should participate as the equals of men in all medical specialties using identical methods, values and insights. In the Soviet Union although the majority of medical doctors were women, they were paid less than the mostly male factory workers.
Paris
Paris (France) and Vienna were the two leading medical centers on the Continent in the era 1750–1914.
In the 1770s-1850s Paris became a world center of medical research and teaching. The “Paris School” emphasized that teaching and research should be based in large hospitals and promoted the professionalization of the medical profession and the emphasis on sanitation and public health. A major reformer was Jean-Antoine Chaptal (1756–1832), a physician who was Minister of Internal Affairs. He created the Paris Hospital, health councils, and other bodies.
Louis Pasteur (1822–1895) was one of the most important founders of medical microbiology. He is remembered for his remarkable breakthroughs in the causes and preventions of diseases. His discoveries reduced mortality from puerperal fever, and he created the first vaccines for rabies and anthrax. His experiments supported the germ theory of disease. He was best known to the general public for inventing a method to treat milk and wine in order to prevent it from causing sickness, a process that came to be called pasteurization. He is regarded as one of the three main founders of microbiology, together with Ferdinand Cohn and Robert Koch. He worked chiefly in Paris and in 1887 founded the Pasteur Institute there to perpetuate his commitment to basic research and its practical applications. As soon as his institute was created, Pasteur brought together scientists with various specialties. The first five departments were directed by Emile Duclaux (general microbiology research) and Charles Chamberland (microbe research applied to hygiene), as well as a biologist, Ilya Ilyich Mechnikov (morphological microbe research) and two physicians, Jacques-Joseph Grancher (rabies) and Emile Roux (technical microbe research). One year after the inauguration of the Institut Pasteur, Roux set up the first course of microbiology ever taught in the world, then entitled Cours de Microbie Technique (Course of microbe research techniques). It became the model for numeous research centers around the world named “Pasteur Institutes.”
Vienna
The First Viennese School of Medicine, 1750–1800, was led by the Dutchman Gerard van Swieten (1700–1772), who aimed to put medicine on new scientific foundations – promoting unprejudiced clinical observation, botanical and chemical research, and introducing simple but powerful remedies. When the Vienna General Hospital opened in 1784, it at once became the world’s largest hospital and physicians acquired a facility that gradually developed into the most important research centre. Progress ended with the Napoleonic wars and the government shutdown in 1819 of all liberal journals and schools; this caused a general return to traditionalism and eclecticism in medicine.
Vienna was the capital of a diverse empire and attracted not just Germans but Czechs, Hungarians, Jews, Poles and others to its world-class medical facilities. After 1820 the Second Viennese School of Medicine emerged with the contributions of physicians such as Carl Freiherr von Rokitansky, Josef Škoda, Ferdinand Ritter von Hebra, and Ignaz Philipp Semmelweis. Basic medical science expanded and specialization advanced. Furthermore, the first dermatology, eye, as well as ear, nose, and throat clinics in the world were founded in Vienna. The textbook of ophthalmologist Georg Joseph Beer (1763–1821) Lehre von den Augenkrankheiten combined practical research and philosophical speculations, and became the standard reference work for decades.
Patient, Surrey County Lunatic Asylum, c. 1850–58. The asylum population in England and Wales rose from 1,027 in 1827 to 74,004 in 1900.
From the early nineteenth century, as lay-led lunacy reform movements gained in influence, ever more state governments in the West extended their authority and responsibility over the mentally ill. Small-scale asylums, conceived as instruments to reshape both the mind and behaviour of the disturbed, proliferated across these regions. By the 1830s, moral treatment, together with the asylum itself, became increasingly medicalised and asylum doctors began to establish a distinct medical identity with the establishment in the 1840s of associations for their members in France, Germany, the United Kingdom and America, together with the founding of medico-psychological journals. Medical optimism in the capacity of the asylum to cure insanity soured by the close of the nineteenth century as the growth of the asylum population far outstripped that of the general population. Processes of long-term institutional segregation, allowing for the psychiatric conceptualisation of the natural course of mental illness, supported the perspective that the insane were a distinct population, subject to mental pathologies stemming from specific medical causes.[136] As degeneration theory grew in influence from the mid-nineteenth century, heredity was seen as the central causal element in chronic mental illness, and, with national asylum systems overcrowded and insanity apparently undergoing an inexorable rise, the focus of psychiatric therapeutics shifted from a concern with treating the individual to maintaining the racial and biological health of national populations.
Emil Kraepelin (1856–1926) introduced new medical categories of mental illness, which eventually came into psychiatric usage despite their basis in behavior rather than pathology or etiology. Shell shock among frontline soldiers exposed to heavy artillery bombardment was first diagnosed by British Army doctors in 1915. By 1916, similar symptoms were also noted in soldiers not exposed to explosive shocks, leading to questions as to whether the disorder was physical or psychiatric. In the 1920s surrealist opposition to psychiatry was expressed in a number of surrealist publications. In the 1930s several controversial medical practices were introduced including inducing seizures (by electroshock, insulin or other drugs) or cutting parts of the brain apart (leucotomy or lobotomy). Both came into widespread use by psychiatry, but there were grave concerns and much opposition on grounds of basic morality, harmful effects, or misuse.
In the 1950s new psychiatric drugs, notably the antipsychotic chlorpromazine, were designed in laboratories and slowly came into preferred use. Although often accepted as an advance in some ways, there was some opposition, due to serious adverse effects such as tardive dyskinesia. Patients often opposed psychiatry and refused or stopped taking the drugs when not subject to psychiatric control. There was also increasing opposition to the use of psychiatric hospitals, and attempts to move people back into the community on a collaborative user-led group approach (“therapeutic communities”) not controlled by psychiatry. Campaigns against masturbation were done in the Victorian era and elsewhere. Lobotomy was used until the 1970s to treat schizophrenia. This was denounced by the anti-psychiatric movement in the 1960s and later.
20th century and beyond
The ABO blood group system was discovered in 1901, and the Rhesus blood group system in 1937, facilitating blood transfusion.
During the 20th century, large-scale wars were attended with medics and mobile hospital units which developed advanced techniques for healing massive injuries and controlling infections rampant in battlefield conditions. During the Mexican Revolution (1910-1920), General Pancho Villa organized hospital trains for wounded soldiers. Boxcars marked Servicio Sanitario (“sanitary service”) were re-purposed as surgical operating theaters and areas for recuperation, and staffed by up to 40 Mexican and U.S. physicians. Severely wounded soldiers were shuttled back to base hospitals. Canadian physician Norman Bethune, M.D. developed a mobile blood-transfusion service for frontline operations in the Spanish Civil War (1936-1939), but ironically, he himself died of blood poisoning.Thousands of scarred troops provided the need for improved prosthetic limbs and expanded techniques in plastic surgery or reconstructive surgery. Those practices were combined to broaden cosmetic surgery and other forms of elective surgery.
During the First World War, Alexis Carrel and Henry Dakin developed the Carrel-Dakin method of treating wounds with an irrigation, Dakin’s solution, a germicide which helped prevent gangrene.
The Great War spurred the usage of Roentgen’s X-ray, and the electrocardiograph, for the monitoring of internal bodily functions. This was followed in the inter-war period by the development of the first anti-bacterial agents such as the sulpha antibiotics.
Public health
Public health measures became particular important during the 1918 flu pandemic, which killed at least 50 million people around the world.[148] It became an important case study in epidemiology. Bristow shows there was a gendered response of health caregivers to the pandemic in the United States. Male doctors were unable to cure the patients, and they felt like failures. Women nurses also saw their patients die, but they took pride in their success in fulfilling their professional role of caring for, ministering, comforting, and easing the last hours of their patients, and helping the families of the patients cope as well.
From 1917 to 1923, the American Red Cross moved into Europe with a battery of long-term child health projects. It built and operated hospitals and clinics, and organized antituberculosis and antityphus campaigns. A high priority involved child health programs such as clinics, better baby shows, playgrounds, fresh air camps, and courses for women on infant hygiene. Hundreds of U.S. doctors, nurses, and welfare professionals administered these programs, which aimed to reform the health of European youth and to reshape European public health and welfare along American lines.
Women had always served in ancillary roles, and as midwives and healers. The professionalization of medicine forced them increasingly to the sidelines. As hospitals multiplied they relied in Europe on orders of Roman Catholic nun-nurses, and German Protestant and Anglican deaconesses in the early 19th century. They were trained in traditional methods of physical care that involved little knowledge of medicine. The breakthrough to professionalization based on knowledge of advanced medicine was led by Florence Nightingale in England. She resolved to provide more advanced training than she saw on the Continent. At Kaiserswerth, where the first German nursing schools were founded in 1836 by Theodor Fliedner, she said, “The nursing was nil and the hygiene horrible.”
The discipline of surgery was put on a sound, scientific footing during the Age of Enlightenment in Europe (1715–89). An important figure in this regard was the Scottish surgical scientist (in London) John Hunter (1728–1793), generally regarded as the father of modern scientific surgery.[43] He brought an empirical and experimental approach to the science and was renowned around Europe for the quality of his research and his written works. Hunter reconstructed surgical knowledge from scratch; refusing to rely on the testimonies of others he conducted his own surgical experiments to determine the truth of the matter. To aid comparative analysis, he built up a collection of over 13,000 specimens of separate organ systems, from the simplest plants and animals to humans.
Hunter greatly advanced knowledge of venereal disease and introduced many new techniques of surgery, including new methods for repairing damage to the Achilles tendon and a more effective method for applying ligature of the arteries in case of an aneurysm.[44] He was also one of the first to understand the importance of pathology, the danger of the spread of infection and how the problem of inflammation of the wound, bone lesions and even tuberculosis often undid any benefit that was gained from the intervention. He consequently adopted the position that all surgical procedures should be used only as a last resort.[45]
Hunter’s student Benjamin Bell (1749–1806) became the first scientific surgeon in Scotland, advocating the routine use of opium in post-operative recovery, and counseling surgeons to “save skin” to speed healing; his great-grandson Joseph Bell (1837–1911) became the inspiration for Arthur Conan Doyle’s literary hero Sherlock Holmes.
Other important 18th- and early 19th-century surgeons included Percival Pott (1714–1788), who first described tuberculosis on the spine and first demonstrated that a cancer may be caused by an environmental carcinogen after he noticed a connection between chimney sweep’s exposure to soot and their high incidence of scrotal cancer. Astley Paston Cooper (1768–1841) first performed a successful ligation of the abdominal aorta. James Syme (1799–1870) pioneered the Symes Amputation for the ankle joint and successfully carried out the first hip disarticulation. Dutch surgeon Antonius Mathijsen invented the Plaster of Paris cast in 1851.
Other important 18th- and early 19th-century surgeons included Percival Pott (1714–1788), who first described tuberculosis on the spine and first demonstrated that a cancer may be caused by an environmental carcinogen after he noticed a connection between chimney sweep’s exposure to soot and their high incidence of scrotal cancer. Astley Paston Cooper (1768–1841) first performed a successful ligation of the abdominal aorta. James Syme (1799–1870) pioneered the Symes Amputation for the ankle joint and successfully carried out the first hip disarticulation. Dutch surgeon Antonius Mathijsen invented the Plaster of Paris cast in 1851.
Modern pain control through anesthesia was discovered in the mid-19th century. Before the advent of anesthesia, surgery was a traumatically painful procedure and surgeons were encouraged to be as swift as possible to minimize patient suffering. This also meant that operations were largely restricted to amputations and external growth removals.
Beginning in the 1840s, surgery began to change dramatically in character with the discovery of effective and practical anaesthetic chemicals such as ether, first used by the American surgeon Crawford Long(1815–1878), and chloroform, discovered by James Young Simpson (1811–1870) and later pioneered in England by John Snow (1813–1858), physician to Queen Victoria, who in 1853 administered chloroform to her during childbirth, and in 1854 disproved the miasma theory of contagion by tracing a cholera outbreak in London to an infected water pump. In addition to relieving patient suffering, anaesthesia allowed more intricate operations in the internal regions of the human body. In addition, the discovery of muscle relaxants such as curare allowed for safer applications. American surgeon J. Marion Sims(1813–83) received credit for helping found Gynecology, but later was criticized for failing to use anesthesia on African test subjects.
The introduction of anesthetics encouraged more surgery, which inadvertently caused more dangerous patient post-operative infections. The concept of infection was unknown until relatively modern times. The first progress in combating infection was made in 1847 by the Hungarian doctor Ignaz Semmelweis who noticed that medical students fresh from the dissecting room were causing excess maternal death compared to midwives. Semmelweis, despite ridicule and opposition, introduced compulsory handwashing for everyone entering the maternal wards and was rewarded with a plunge in maternal and fetal deaths, however the Royal Society dismissed his advice.
Until the pioneering work of British surgeon Joseph Lister in the 1860s, most medical men believed that chemical damage from exposures to bad air (see “miasma”) was responsible for infections in wounds, and facilities for washing hands or a patient’s wounds were not available.[47] Lister became aware of the work of French chemist Louis Pasteur, who showed that rotting and fermentation could occur under anaerobic conditions if micro-organisms were present. Pasteur suggested three methods to eliminate the micro-organisms responsible for gangrene: filtration, exposure to heat, or exposure to chemical solutions. Lister confirmed Pasteur’s conclusions with his own experiments and decided to use his findings to develop antiseptic techniques for wounds. As the first two methods suggested by Pasteur were inappropriate for the treatment of human tissue, Lister experimented with the third, spraying carbolic acid on his instruments. He found that this remarkably reduced the incidence of gangrene and he published his results in The Lancet. Later, on 9 August 1867, he read a paper before the British Medical Association in Dublin, on the Antiseptic Principle of the Practice of Surgery, which was reprinted in The British Medical Journal.[51] His work was groundbreaking and laid the foundations for a rapid advance in infection control that saw modern antiseptic operating theatres widely used within 50 years.
Lister continued to develop improved methods of antisepsis and asepsis when he realised that infection could be better avoided by preventing bacteria from getting into wounds in the first place. This led to the rise of sterile surgery. Lister instructed surgeons under his responsibility to wear clean gloves and wash their hands in 5% carbolic solution before and after operations, and had surgical instruments washed in the same solution.[52] He also introduced the steam steriliser to sterilize equipment. His discoveries paved the way for a dramatic expansion to the capabilities of the surgeon; for his contributions he is often regarded as the father of modern surgery.[53] These three crucial advances – the adoption of a scientific methodology toward surgical operations, the use of anaesthetic and the introduction of sterilised equipment – laid the groundwork for the modern invasive surgical techniques of today.
In the late 19th century William Stewart Halstead (1852–1922) laid out basic surgical principles for asepsis known as Halsteads principles. Halsted also introduced the latex medical glove. After one of his nurses suffered skin damage due to having to sterilize her hands with carbolic acid, Halsted had a rubber glove that could be dipped in carbolic acid designed.
The use of X-rays as an important medical diagnostic tool began with their discovery in 1895 by German physicist Wilhelm Röntgen. He noticed that these rays could penetrate the skin, allowing the skeletal structure to be captured on a specially treated photographic plate.
In the past century, a number of technologies have had a significant impact on surgical practice. These include Electrosurgery in the early 20th century, practical Endoscopy beginning in the 1960s, and Laser surgery, Computer-assisted surgery and Robotic surgery, developed in the 1980s.
Cardiac surgery was revolutionized in the 1948 as open-heart surgery was introduced for the first time since 1925.
In 1954 Joseph Murray, J. Hartwell Harrison and others accomplished the first kidney transplantation. Transplantations of other organs, such as heart, liver and pancreas, were also introduced during the later 20th century. The first partial face transplant was performed in 2005, and the first full one in 2010. By the end of the 20th century, microtechnology had been used to create tiny robotic devices to assist microsurgery using micro-video and fiber-optic cameras to view internal tissues during surgery with minimally invasive practices.[157]Laparoscopic surgery was broadly introduced in the 1990s. Natural orifice surgery has followed. Remote surgery is another recent development, with the Lindbergh operation in 2001 as a groundbreaking example.
Twitter feed is currently turned off. You may turn it on and set the API Keys and Tokens using Theme Options -> Social Options: Enable Twitter Feed.